Sara Qureshi BDS
Muhammad Waseem Ullah Khan BDS, FCPS, CMT
Momina Akram BDS, FCPS
of ectodermal dysplasia most often requires a multidisciplinary approach to achieve desired cosmetic results. This case report
illustrates Prosthodontic rehabilitation of a 20-year-old female patient having oligodontia associated with ectodermal dysplasia
and severe skeletal class III malocclusion with the chief complaint of unpleasant esthetics and poor masticatory function. She
had multiple missing teeth and a malformed appearance of the remaining teeth with deranged occlusion. The patient was
rehabilitated with a combination of fixed and removeable prosthodontics thereby evidently enhancing the esthetic and functional
outcome.
KEYWORDS: Rehabilitation, ectodermal dysplasia, hypodontia, skeletal class III.
HOW TO CITE: Qureshi S, Khan MWU, Akram M. Oral Rehabilitation of Ectodermal dysplasia associated hypodontia in an
adolescent patient with skeletal class III. J Pak Dent Assoc 2024;33(1):27-31.
DOI:https://doi.org/10.25301/JPDA.331.27
Received:10 December 2023, Accepted: 23 March 2024
INTRODUCTION
Ectodermal Dysplasia (ED) is a rare heterogenous group of genetic disorders primarily attributed to the mutational changes in the genes which encode for the development of embryonic ectodermal structures and their appendages; skin, nails, teeth, hair and eccrine glands.1 Since ectodermal dysplasias have a genetic etiology, they commonly follow a mendelian inheritance pattern. However, it has been conjectured that they can also occur in individuals with no previous family history where a de novo mutation might have occurred.
Skimming through the literature divulged that approximately, more than 200 different types of ectodermal dysplasias have been identified till this date.3 Ectodermal dysplasia can be broadly classified into hypohidrotic and hidrotic forms based upon the clinical manifestations of the syndrome.4 Hypohidrotic ectodermal dysplasia (HED 1) also known as Christ-Siemens-Touraine Syndrome is the most common variant of ED, which is characterized by the expression of hypohidrosis, hypodontia or anodontia and hypotrichosis .5 The genetic pathogenesis of this form is described by the mutations in the EDA gene which presents an X-linked recessive mode of inheritance thereby predominantly affecting males.6 However, X-linked carrier females exhibit an intermediate expression in the form of mild hypodontia and spottily reduced sweating. The hidrotic type (HED 2) is also known as Clouston syndrome which is inherited as an autosomal dominant disorder. It exhibits a phenotypical triad of nail dystrophy, palmoplantar hyperkeratosis and patchy alopecia with normal dentition and eccrine glands.
Dental manifestations of ectodermal dysplasia are characterized by conical, peg-shaped malformed teeth, hypodontia or complete anodontia of primary or permanent teeth with accompanying skeletal discrepancies which can be a cause of great esthetic concern for the patient.7 Literature has been very generous in unfolding a variety of treatment modalities for these patients and has time and again advocated an early intervention based on a multidisciplinary approach for their successful rehabilitation.
This clinical report aims to illustrate the Prosthodontic rehabilitation of an adolescent patient having oligodontia associated with ectodermal dysplasia and severe skeletal class III malocclusion
CLINICAL REPORT
A 20-year-old female patient reported to the outpatient Department of Prosthodontics de ‘Montmorency College of Dentistry, Lahore with the chief complaint of unpleasant aesthetics and difficulty in mastication due to deranged occlusion, multiple missing teeth and conical malformed appearance of remaining teeth with wide spacing between them (Figure 1a). Detailed medical and dental history revealed

extraction of grossly carious deciduous mandibular left first and second molar almost six months ago. However, the medical history was insignificant. Family history revealed normal parents with a consanguineous marriage. Two of her thirteen siblings and a few of her maternal relatives had the same dental problem which was indicative of a mendelian inheritance pattern.
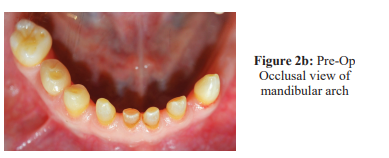
Intraoral examination of the patient evinced the presence of retained deciduous dentition with congenital absence of maxillary lateral incisors and multiple missing permanent teeth (Figure 2a). The existing teeth were small, peg shaped, malformed microdonts. A unilateral free-end saddle area

(Kennedy class II) was present distal to mandibular left canine (Figure 2b). She had a skeletal class III maxillomandibular relationship with an anterior and right posterior crossbite. A forward and upward displacement of mandible was observed with a complete loss of anterior guidance and an anterior negative overjet of -3mm was recorded. The freeway space was measured to be 8mm. Soft tissue evaluation of mucosa, tongue and gingiva revealed normal color and texture. Oral hygiene status was satisfactory.
Panoramic radiograph of the patient showed poor crown-toroot ratios for deciduous maxillary and mandibular incisors (Figure 2c). There was complete anodontia of permanent

dentition as no signs of impacted or unerupted permanent teeth were found in the jaws.
Thorough clinical and radiographic evaluation led to the diagnosis of oligodontia associated with hypohidrotic ectodermal dysplasia. Diagnostic casts were obtained using alginate hydrocolloids to work out for a viable treatment plan. Since the Patient desired for complete arch fixed reconstructions, further diagnostic imaging with a CBCT was done for the 3-D analysis of maxillary and mandibular bone to determine any possibility of implant placement. Regrettably CBCT analysis revealed hypoplasia of the alveolar bone structure with inadequate bone volume at the prospective implant sites. Autogenous bone grafting could not be done due to the potential risks of morbidity and financial constraints associated with it. Hence the consideration for implant placement was laid aside.
After a meticulous discussion with the patient regarding the limitations of various treatment options, a combination of fixed and removeable Prosthodontics was deemed to be the most befitting treatment plan in the present case scenario. A removeable cast partial denture to replace the four maxillary incisors with individual surveyed crowns on remaining teeth to restore their height and shape was planned for the maxillary arch. Likewise, a removeable cast partial denture was planned for the mandibular arch to replace the four incisors and the free-end-saddle area along with individual surveyed crowns.
on the remaining teeth in the arch. Deciduous maxillary central incisors and mandibular central and lateral incisors with poor crown-to-root ratios were not extracted, rather it was decided to preserve them as over denture abutments after their elective endodontics. Prior to beginning the treatment, written informed consent was taken from the patient for the publication of this case report.
CLINICAL PROCEDURE
Maxillary and mandibular diagnostic impressions were taken in an alginate hydrocolloid. A free way space of 8mm was recorded after determining the discrepancy between resting vertical dimension (RVD)and occlusal vertical dimension (OVD) on the patient. Facebow transfer record of the patient was taken and diagnostic casts were mounted using a centric relation record on a semi adjustable Arcon type articulator. A 4mm increase in the occlusal vertical dimension was planned thus evenly distributing a 2mm increase for each arch. As the patient desired an early restoration of maxillary arch for the purpose of improving the esthetic smile line, it was decided to first restore the maxillary arch and then mandibular arch was restored accordingly.
MAXILLARY ARCH REHABILITATION
Diagnostic wax up was done on the articulated maxillary cast such that the existing three teeth on each side of the arch were contoured as canine, 1st premolar and 1st molar (Figure 3a, 3b). Thermoplastic vacuum-formed template was fabricated after the duplication of waxed-up maxillary

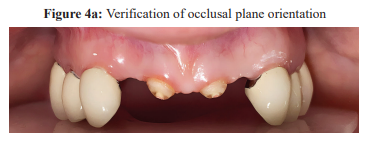
cast to facilitate the intra oral mockup and composite build ups. An intra oral mockup of maxillary arch was done with an auto polymerizing acrylic resin to validate the position of esthetic plane of occlusion which was found to be appropriate relative to the patient’s interpupillary line and facial proportions. After the esthetic verification, the mockup was removed, and composite buildups of maxillary teeth were done to restore their height and shape prior to their crown preparations. The patient was recalled after two weeks and her adaptation to increased occlusal vertical dimension was evaluated, for which she reported no pain or discomfort. Tooth preparations were carried out conservatively with vertical finish lines (knife edge, feather edge) to allow for the enamel preservation in the cervical area. Final impression of the preparations was taken in an addition silicon impression material by employing a dual phase two step technique. Facebow transfer and jaw relation records were repeated and sent to the laboratory for the fabrication of porcelain fused to metal surveyed crowns on the prepared abutments. Provisional crowns were cemented while the definitive restorations were being fabricated. Prior to the final delivery of surveyed crowns, they were tried in with Cavit Provis to verify esthetics and occlusal plane orientation (Figure 4a). A fox’s bite plane was used to check for the parallelism between campers’ plane and occlusal plane. Definitive
surveyed crowns were cemented with glass ionomer luting cement. Meanwhile elective endodontics of maxillary central incisors were carried out and they were subsequently prepared to have a dome shaped contour, only 1mm above the gingival margin to serve as overdenture abutments (Figure 4b). A Scandinavian design was chosen for maxillary cast partial denture. The final impression for the cast partial denture

was taken in an alginate irreversible hydrocolloid impression material which was then sent to laboratory for framework fabrication. The cast metal framework try inn was done to ensure adequate marginal adaptation. Processed maxillary
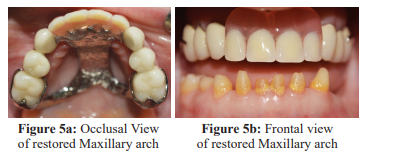
cast partial denture replacing the four incisors was insertedat the subsequent appointment (Figure 5a, 5b).
MANDIBULAR ARCH REHABILITATION
Enameloplasty of the facial surfaces of mandibular left canine, right second deciduous molar was done after their elective endodontics, so that future crowns can be fabricated with a slight lingual inclination to eliminate the existing anterior crossbite and possibly reduce the posterior crossbite. A diagnostic impression of mandibular arch and a pick-up impression of the restored maxillary arch was taken in an alginate impression material. The maxillary and mandibular casts were rearticulated at the planned occlusal vertical dimension using a facebow transfer and centric relation record. Diagnostic wax-up on the articulated mandibular cast was done (Figure 6a, 6b). Composite build ups of mandibular teeth were done prior to their crown preparations

as had been previously done for maxillary arch using a clear vacuum formed template. The patient was recalled after one week to evaluate the adaptation to increased vertical dimension of occlusion. Afterwards, conservative vertical crown preparations were carried out and a dual phase two step impression of the prepared teeth was taken in an addition silicone elastomeric impression material. Jaw relation records were repeated and sent to laboratory for the fabrication of porcelain fused to metal surveyed crowns. Prior to the cementation of final prostheses with glass ionomer cement, occlusion was adjusted with the help of an articulating paper such that class I canine relationship was achieved on both sides of the arch (Figure 7a, 7b). Mandibular central and lateral incisors were prepared as overdenture abutments after their elective endodontics (Figure 8a). The impression for the cast partial denture was taken using the selective pressure


impression technique. The distal extension region was recorded in impression compound and final wash impression was taken in alginate impression material which was then sent to laboratory for framework fabrication. After the try inn of the cast metal framework, the tooth setup was done such that anterior teeth were retroclined to eliminate anterior cross bite. Moreover, they were ground to thin veneers due to the limited interarch space availability. The processed mandibular cast partial denture was inserted, and patient was evaluated for esthetics, phonetics and mastication

DISCUSSION
Implants have not always been a very predictable treatment modality in ectodermal dysplasia patients with severely reduced alveolar bone volume. As in these patients, invasive bone augmentation procedures are often deemed necessary for implant placement in a prosthetically driven position.9 Consequently, extensive bone augmentation has its own possible repercussions; tissue dehiscence, graft exposure which ultimately leads to augmentation failure. As the perpetual preservation of what remains is more important than the meticulous replacement of what is missing, therefore in this clinical case a less invasive approach was employed to preserve the alveolar ridge by retaining the natural teeth with poor crown to root ratios as over denture abutments instead of extracting them. Moreover, remaining teeth were restored with individual crowns due to their better prognosis when contrasted with fixed partial dentures.
The loss of occlusal vertical dimension is a common finding in patients presenting with ectodermal dysplasia .11 Hence determining the tolerance for the planned increase in occlusal vertical dimension is of paramount importance prior to beginning any irreversible treatment. Contemporary literature advocates that there is no well-defined time frame to assess the tolerance for an increased occlusal vertical dimension and it is based on patient’s subjective perception of comfort.12 In the present clinical scenario, the occlusal vertical dimension was sequentially raised to slowly improve the tolerance to increased vertical dimension. The adaptation to raised occlusal vertical dimension was evaluated after two weeks of composite build ups and fortunately the patient reported no muscle fatigue or pain in temporomandibular joint.
Interpupillary line and ala-tragus line (Camper’s plane) are regarded as reliable facial references for an esthetic dental reconstruction.13 The esthetic occlusal plane of the underdiscussion patient was verified by determining the parallelism of maxillary occlusal plane to interpupillary line anteriorly and ala-tragus line posteriorly. The patient’s esthetic perception was given a significant weight while selecting the shade of artificial teeth. A lighter shade was chosen to harmonize with the corresponding fair complexion of the patient. Maxillary cast partial denture was designed by employing a Scandinavian approach which leaves the gingival margins of remaining teeth exposed and devoid of any major connector coverage to prevent any hindrance to mouth’s self-cleansing ability.14 Thereby extracting the biological benefits of maintaining gingival health and limiting the buildup of plaque. For mandibular cast partial denture, a lingual plate was the major connector of choice to provide indirect retention in the presence of a distal extension base.
CONCLUSION
Oral rehabilitation of ectodermal dysplasia with a skeletal class III discrepancy presents an arduous challenge to dentists around the world. However early prosthodontic intervention is cardinal to prevent the long-term sequelae. The aforementioned hybrid rehabilitation with fixed and removeable prosthodontics gave a successful esthetic and functional outcome. Thereby positively building the social confidence and self-esteem of the patient.
CONFLICT OF INTEREST
None declared
REFERENCES
- Wright JT, Fete M, Schneider H, Zinser M, Koster MI, Clarke AJ, et al. Ectodermal dysplasias: Classification and organization by phenotype, genotype and molecular pathway. Am J Med Genetics Part A. 2019;179:442-7. https://doi.org/10.1002/ajmg.a.610457
- . Modesto A, Ventura C, Deeley K, Studen-Pavlovich D, Vieira AR. Medical sequencing of de novo ectodermal dysplasia in identical twins and evaluation of the potential eligibility for recombinant EDA therapy. J Dent Res, Dental Clinics, Dental Prospects. 2017;11:135-9. https://doi.org/10.15171/joddd.2017.025
- Grange DK. Ectodermal Dysplasias. Elsevier eBooks. 2013;1-26. https://doi.org/10.1016/B978-0-12-383834-6.00157-9
- Grover R, Mehra M. Prosthodontic Management of Children with Ectodermal Dysplasia: Review of Literature. Dentistry. 2015;5. https://doi.org/10.4172/2161-1122.1000340
- Pigno MA, Blackman RK, Cronin RM, Cavazos E. Prosthodontic management of ectodermal dysplasia: A review of the literature. The J Prosthetic Dentist. 1996;76:541-5. https://doi.org/10.1016/S0022-3913(96)90015-3
- Deshmukh S, Prashanth S. Ectodermal Dysplasia: A Genetic Review. Int J Clinical Pediatric Dentist. 2012;5:197-202 https://doi.org/10.5005/jp-journals-10005-1165
- Van Sickels JE, Raybould TP, Hicks EP. Interdisciplinary Management of Patients With Ectodermal Dysplasia. J Oral Implantol. 2010;36:239-45. https://doi.org/10.1563/AAID-JOI-D-09-00043R1
- Alajami H, Saker J. Rehabilitation of ectodermal dysplasia patient with a telescopic denture in the maxilla and mandibular implant assisted overdenture: A case report. Clinical Case Reports. 2021;9. https://doi.org/10.1002/ccr3.5206
- El Charkawi H, Barakat A, Alm Eldean HI. Full mouth implants rehabilitation of a patient with ectodermal dysplasia after 3-Ds ridge augmentation. A clinical report. Future Dent J. 2016;2:4-14. https://doi.org/10.1016/j.fdj.2016.02.002
- Misch CE. Rationale for Dental Implants *. Elsevier eBooks. 2015;1- 25. https://doi.org/10.1016/B978-0-323-07845-0.00001-4
- . Koyuncuoglu CZ, Metin S, Saylan I, Calisir K, Tuncer O, Kantarci A. Full-Mouth Rehabilitation of a Patient With Ectodermal Dysplasia With Dental Implants. Journal of Oral Implantology. 2014 Dec 1;40:714-21. https://doi.org/10.1563/AAID-JOI-D-12-00072
- Vailati F, Urs S, Belser C. Full-Mouth Adhesive Rehabilitation of a Severely Eroded Dentition: The Three-Step Technique. Part 2. THE European J Esthetic Dentist. 2008;3.
- Sabbah A. Smile Analysis. Dental Clinics of North America. 2022;66:307-41. https://doi.org/10.1016/j.cden.2022.03.001
- . Berg E, Isidor FI, Öwall B. Prosthodontics for the elderly patient – a Scandinavian approach. Prosthodontics. 2018 Aug 15;68(3):255-66. https://doi.org/10.5604/01.3001.0012.2556